Health Services
Health services are essential in schools to ensure students are receiving both preventive and needed care for their potential and current health problems. Health services connect school staff, students, families, community and healthcare providers to promote the health care of students and a healthy and safe school environment. School health services actively collaborate with school and community support services to increase the ability of students and families to adapt to health and social stressors, such as chronic health conditions or social and economic barriers to health, and to be able to manage these stressors and advocate for their own health and learning needs.
When it comes to providing preventive care, school health services have a duty to communicate effectively and educate students and their families on key topics such as BMI and immunization requirements.
Adapted from www.cdc.gov/whole-school-community-child/about/index.html
-
School Nurse Professional Development Web Series
Penn State PRO Wellness, in collaboration with Highmark Foundation, is pleased to offer no-cost, pre-recorded professional development opportunities for school nurses.
In an effort to improve school health, PRO Wellness surveyed school nurses to gain insight into which educational topics would be of most value to them and their schools. Using the information collected, PRO Wellness developed five pre-recorded, professional development trainings for school nurses. Physician experts from Penn State Health Milton S. Hershey Medical Center and Allegheny Health Network were consulted to create topical trainings.
NOTE: We are no longer able to provide access to ACT 48/58 credit hours for completion of the pre-recorded, school nurse professional development trainings. However, we will issue a certificate of completion. Click here to request a certificate of completion that can be submitted through your professional channels to request credit.
Topics include:
BMI Toolkit
Penn State PRO Wellness has developed this Body Mass Index (BMI) Toolkit to assist school nurses, pediatricians and other qualified health services providers with effective BMI screening.
The information contained in this toolkit is intended to provide resources to assist in communicating with students and their families to help them understand their BMI, and behaviors that promote a healthy lifestyle. Our recommended BMI screening letter is just one of the many tools offered.
-
What is Body Mass Index (BMI)?
Body Mass Index (BMI) is a useful screening tool that can serve as a measure of body fat and uncover potential weight and health-related issues.
There are many factors that determine an individual’s BMI, weight and body fat. This includes genetics and family history, environmental factors and daily lifestyle choices. While factors like family history cannot be changed, there are many simple ways to bring healthy choices to life in order to reduce your risk for health problems and disease.
Children and adolescents who screen as overweight or obese are at greater risk for developing serious health diseases and conditions such diabetes, high blood pressure, heart disease, bone and joint problems and sleep apnea.
A growing concern among experts is that for the first time in U.S. history, the current generation will live shorter, unhealthier lives than their parents due to the obesity epidemic.
Obesity affects about 12.7 million U.S. children and adolescents. Despite recent declines in the prevalence among preschool-aged children, obesity among children is still too high, hovering around 17% for ages 2 – 19.
Students in Pennsylvania are screened for BMI as part of annual, state-mandated health screenings in schools. Although BMI screenings and notification programs hold promise of addressing a serious issue, a gap still exists in follow-up measures for children who screen overweight and obese.
Parents value weight-focused guidance from a trusted medical professional. Research has shown that patients who were counseled in a primary care setting about the benefits of healthy eating and physical activity often took positive action. Patients lost weight and exercised more than peers who did not receive counseling. Parents are more likely to identify their child’s correct body image and address unhealthy behaviors after conversations with their pediatrician.
Original Sources
- Prevention CfDCa. Childhood Obesity Facts | Overweight & Obesity | CDC2016.
- Ogden CL, National Center for Health Statistics UCfDCaP, Hyattsville, Maryland, Carroll MD, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988-1994 Through 2013-2014. JAMA. 2016;315:2292-2299.
- NIH. Talking with Patients about Weight Loss: Tips for Primary Care Providers 2016.
- Hernandez RG, Cheng TL, Serwint JR. Parents’ Healthy Weight Perceptions and Preferences Regarding Obesity Counseling in Preschoolers: Pediatricians Matter. 2010.
-
What is BMI-for-age?
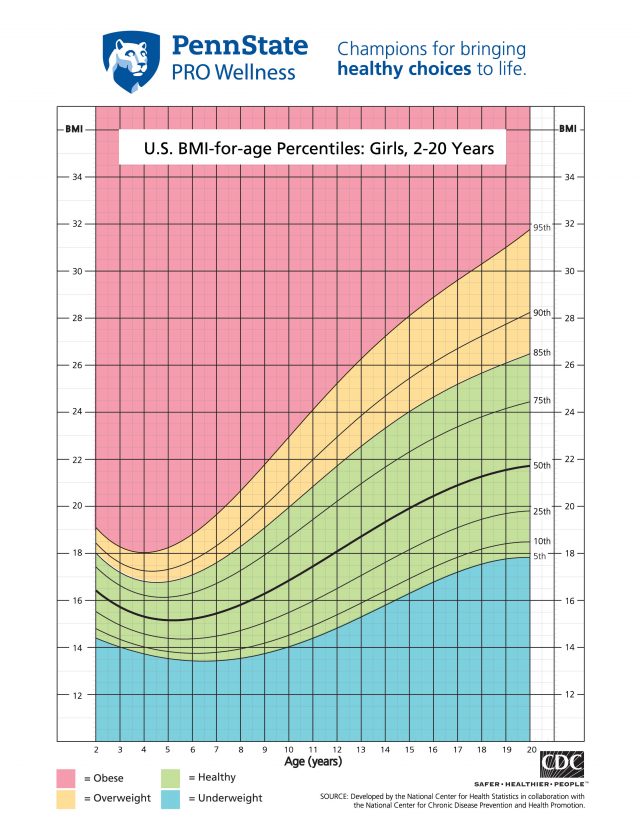
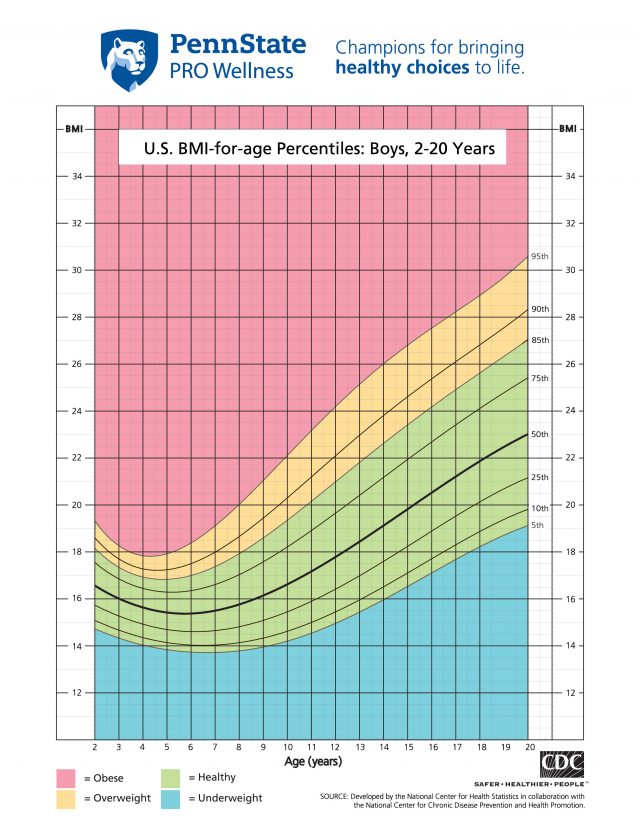
BMI for children and young adults ages 2-19 is referred to as BMI-for-age. The reason for this is that body fat changes as you grow. BMI-for-age is plotted on separate growth charts to determine a BMI percentile ranking.
A BMI percentile is an indication of how a child’s measurements compare to others of the same age and gender. A child whose BMI is at the 50th percentile is close to the average of the population. A child above the 95th percentile is considered obese because 95 percent of the population weighs less than he or she does. A child below the 5th percentile is considered underweight because 95 percent of the population weighs more. You may receive these charts at your child’s yearly checkup.
Child Percentile
- Less than 5th percentile: underweight
- 5th to less than 85th percentile: healthy weight
- 85th to less than 95th percentile: overweight
- Equal to or greater than 95th percentile: obese
Use this calculator to calculate BMI and the corresponding BMI-for-age percentile based on the CDC growth charts for children and teens (ages 2 through 19 years).
-
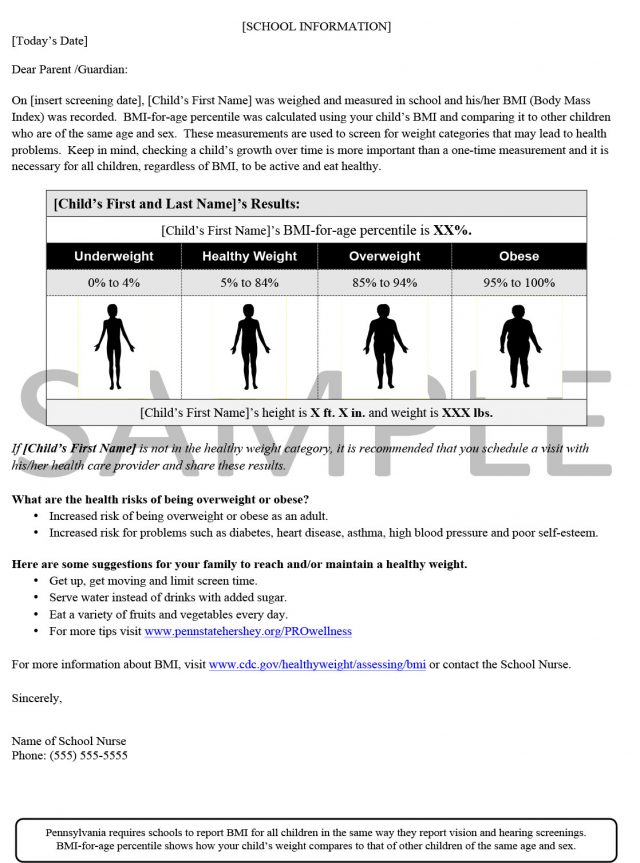
Request Recommended BMI Screening Letter
Studies show that school-based interventions have been unsuccessful in reducing childhood obesity prevalence, potentially due to the lack of follow-up with appropriate nutritional education programming. To help fill this gap, the Highmark Foundation partnered with Penn State PRO Wellness to develop and test an effective BMI screening letter that leads parents to digital tools and resources for making healthy lifestyle changes for their families. This letter is now recommended for use by the Pennsylvania Department of Health.
Our research team was pleased to learn that this revised letter showed favorable results. Among parents of overweight or obese children, more recipients of the revised letter intended to take action based on information it contained when compared to those receiving the standard letter (68% vs. 45%). In addition, parents of overweight or obese children who received the revised as compared to the standard letter were more likely to read the entire letter (82% vs. 77%).
Click here to complete the BMI Screening Letter request form, be sure to select ‘BMI Letter’ from the selection options. Once your information is received, you will gain access to our BMI Letter via email.
-
BMI Counseling Provider Tools
Unhealthy habits can be difficult to break but possible to change. Consistent, progressive steps to making wise food choices and increasing physical activity are the two most important steps to achieving a healthy weight. Small changes can add up to huge benefits and can be as easy as updating recipe ingredients with healthier options. Suggestions on moving more can be as simple as taking a brisk 30-minute walk after a meal. Gradual changes are more likely to become lifestyle habits over time.
Opening up a discreet and sensitive dialog with patients can improve efforts to motivate them to make healthy lifestyle changes. Approach weight-related concerns with privacy and without judgment, this can be done by asking if it’s okay to talk about wellness goals. Children and parents may be more receptive and feel less threatened.
No one wants to be singled out when it comes to his or her weight. Suggest team-oriented or family activities to encourage healthful changes. Family and friends can support one another by cooking, eating and moving together. These activities can put children at ease and give them the boost needed to form healthier habits.
Share the following resources to guide families on making healthy food and activity choices.
- Penn State PRO Wellness Recipes
- Healthy Choices: Eating Healthy on a Budget
- Healthy Choices: Energy Balance
- Healthy Choices: Cooking, Kid Approved
- Healthy Choices: Snack Swaps
- Healthy Choices: Portion Distortion
- Healthy Choices: Rethink Your Drink
- Healthy Choices: Daily Breakfast Tips
- Healthy Choices: Setting Wellness Goals
- Healthy Choices: Getting a Good Night’s Sleep
- Healthy Choices: Family Exercise without Equipment
For School Nurses
School nurses are in a key position to address the needs of children who are obese and overweight as well as advocate for those at risk of becoming obese. Students see you regularly and look to your expertise. Parents know if a health crisis occurs, you are there to ensure their child’s safety and care.
Pennsylvania law mandates yearly school health screenings of height, weight and BMI. Calculated BMI results serve as a tool to identify students who require follow up care.
Poor diet and inadequate physical activity are leading contributors to being overweight and obese. As a trusted medical professional, you can offer guidance on evidenced-based resources and practical solutions to make healthy choices a lifestyle.
Try these strategies:
- Be diligent in notifying parents of BMI screening results. Use the recommended parent-tested BMI letter.
- In addition to the BMI letter, follow up with parents of children who screen overweight or obese.
- Stress to parents the importance of following up with their child’s healthcare provider regarding an unhealthy BMI for further assessment and treatment.
- Use toolkit resources to encourage students and families on:
- A balanced diet can help children grow up healthy. However, it’s not always easy to eat healthy when you’re juggling a busy schedule. Looking for healthy meal options? Our Healthy Champions Recipes portal can help you make wise food choices.
- Become aware of community resources available and make referrals for students needing weight counseling or additional support.
- Work with the school district to improve nutrition and physical activity by providing healthy choices at mealtimes and promoting more physical activity during, before and after school.
- Advocate for nutrition and wellness education programs throughout every grade level.
For Pediatricians
Below you will find additional resources for providing tips, answers and information to patients and families.
Pediatric E-Practice: Optimizing Your Obesity Care (PeP) (a virtual office) is a new and fun way to access resources to support pediatric obesity care. PeP is a virtual office that provides access to the American Academy of Pediatrics and partner resources for prevention, assessment and treatment all in the context of pediatric office workflow.
The Role of the Pediatrician in Primary Prevention of Obesity
Stephen R. Daniels, Sandra G. Hassink
This clinical report describes the rationale for pediatricians to be an integral part of the obesity-prevention effort. This report also identifies important gaps in evidence that need to be filled by future research.Parents’ Healthy Weight Perceptions and Preferences Regarding Obesity Counseling In Preschoolers: Pediatricians Matter
Raquel G. Hernandez, Tina L. Cheng, and Janet R. Serwint
This paper describes a study comparing parental report of child body image with perceived healthy weight body image in preschoolers and discovered that weight focused advice from pediatricians matters to parents and may promote parental identification of early childhood weight risks.Mobile Apps for Providers and Parents
The American Academy of Pediatrics partners with publishers of mobile apps in order to provide both parents and health care providers with tools for fast, convenient answers and information.Institute for Healthy Childhood Weight – Quick links and Resources
The American Academy of Pediatricians Institute of Healthy Childhood Weight will serve as a transitional engine to optimize health care, engage families and catalyze communities. -
Motivational Interviewing: ABC’s of Counseling Overweight Children and Families
Motivational Interviewing (MI) is a well-known, scientifically tested method of counseling clients to make behavioral changes. Its founders, Dr. William R. Miller and Dr. Stephen Rollnick, define it as “a directive, client-centered counseling style for eliciting behavior change by helping clients to explore and resolve ambivalence. Compared with nondirective counseling, it is more focused and goal-directed.” Its use can be an effective tool in helping obese and overweight children.
Finding the best way to talk about the sensitive topic of weight is not always easy. Both patients and parents are often reluctant to discuss weight for fear of shame, blame or judgment. Asking, listening and empowering families to participate actively in making wise choices about their health are key components to MI. Following are some quick tips for communicating with patients.
- Ask open-ended questions
- How do you feel about us talking about your physical activity, TV watching, and eating today?
- How concerned are you about your child’s weight?
- What are some of the things you might like to change?
- Body language
- Put patient(s) at ease.
- Use eye contact without barriers.
- Convey respect.
- Counsel in a private setting.
- Care and Empathy
- Do not criticize.
- Acknowledge patient’s feelings.
- Answer questions without signs of judgment.
- Use language that is nonjudgmental
- “Healthier” food vs “bad” food
- “Healthier” weight vs “ideal” weight
Click here to view a digital skill-building practice tool that helps healthcare providers build MI skills. Engage in a conversation with a virtual mother and her son and apply MI techniques to drive positive change in health behaviors.
Source: Pediatric Obesity Clinical Decision Support Chart. American Academy of Pediatrics
- Ask open-ended questions
-
Weight Management Programs
Children who are overweight or obese and their families who find it hard to establish healthy habits on their own may benefit from a weight management program. Goal setting, accountability by monitoring progress and specialized guidance are components of a more structured program and provide the added support some need to make healthy, long lasting changes.
Many of the following community groups offer free or low-cost nutrition or fitness classes. As a resource to guide patients and families, compile a list of those offered in your area:
- Family community centers
- Senior centers
- Parks and recreation departments
- Local colleges
- Grocery stores
- After school programs
- Churches
Patients should always consult their healthcare providers before starting any weight loss program.
Programs that are more extensive can range from meeting with a nutritionist to seeking a multidisciplinary healthcare team at a weight control center.
- Pediatric Weight Loss Management Program: Doctors and registered dietitians designed the Penn State Children’s Hospital Pediatric Weight Loss Management Program to meet the specific needs of overweight children. Experts help children ages 15 months to 21 years reach their weight loss goals.
- Fit, Trim and Slim Weight Management Program: The Weight Management Program, adult weight loss program at Penn State Heart and Vascular Institute, helps individuals identify factors of weight gain and develop strategies to lose weight. Noted experts in the fields of behavioral modification, nutrition and exercise will develop strategies for losing weight and keeping it off.
- Penn State Health Milton S. Hershey Medical Center Surgical Weight Loss: The comprehensive surgical weight loss program at Penn State Milton S. Hershey Medical Center was started in 1979. The program continues to offer comprehensive weight management services including: nutritional counseling, medical evaluation, psychiatric evaluation, and weight loss surgery (sometimes called stomach stapling or bariatric surgery) for patients with clinically severe obesity.
Immunization Toolkit
Penn State PRO Wellness has developed the Pennsylvania School Nurse Immunization Toolkit to assist Pennsylvania school nurses with achieving immunization compliance across their school(s).
This information is intended to serve as a guide and to provide resources during the academic year to assist in identifying needs, developing an action plan, and implementing sustainable communication methods.
-
Pennsylvania School Vaccination Requirements
Vaccinations are required for children to attend school in Pennsylvania. A new regulation was enacted at the start of the 2017/18 school year reducing the provisional period to zero days for single-dose immunizations and 5 days for multi-dose immunizations. The school immunization regulations are intended to ensure that children attending school in the commonwealth are protected against potential outbreaks of vaccine preventable diseases.
The Pennsylvania Department of Health provides several resources for both parents and schools.
Information for Parents:
- School Vaccination Flyer for Parents
- School Vaccination Requirement Fact Sheet
- Frequently Asked Questions
Information for Schools:
- PA State Law and Regulation
- School Immunization Regulation Procedure Manual
- Certificate of Immunizations
- Medical Certificate
- School Vaccination for School Nurses
- School Immunization Requirements for ALL grades – Dichotomous Key (Algorithm)
- School Immunization Requirements 7th-12th grade – Dichotomous Key (Algorithm 2)
Click here to access additional resources about the School Immunization Law Report (SILR) and the School Immunization Catch-Up Program (SICU) through the Pennsylvania Department of Health.
-
CDC Recommended Immunizations by Age Group
On-time vaccination throughout childhood is essential because it helps provide immunity before children are exposed to potentially life-threatening diseases. Vaccines are tested to ensure that they are safe and effective for children to receive at the recommended ages. Talk to your child’s doctor about the vaccine recommendations for their age.
Click on each age group below to view the CDC recommended vaccination schedules:
- Infants and Children (birth through 6 years old)
- Children (7 through 18 years old)
- Child and Adolescent (ages 18 years or younger)
- Adult (ages 19 years or older)
Additional resources:
-
Immunization Compliance Management Tools
Immunization compliance management and data tracking is just one aspect of a school nurse’s role. In order to track student’s immunization data effectively and timely, school nurses must have an organized plan and the tools needed to implement it.
Penn State PRO Wellness’ research team conducted two studies to learn more about resources needed by school nurses in Pennsylvania. To gain an understanding of current practices and needed resources, we conducted 21 interviews with school nurses who expressed a need for resources to manage the immunization compliance tracking process. A follow-up survey of 350 Pennsylvania school nurses also expressed that their current data tracking process is burdensome (47%) and a need for help to create a streamlined process (36%).
To facilitate creating and implementing a comprehensive immunization compliance management plan, Penn State PRO Wellness has developed a series of templates and resources for school nurses.
-
Immunization Education Resources
Vaccine hesitancy is increasing causing a great threat to public health. A lot of the hesitancy that surrounds vaccines stems from an overwhelming amount of misinformation that is often promoted through social media channels. To combat this misinformation, it’s important to provide families with accurate information so they can make informed decision about their child’s health and well-being.
Use these resources to assist in your communication efforts with families and to promote immunization compliance.
-
Recommended Immunization Compliance Notification Letter
A survey to 350 school nurses across Pennsylvania revealed that 76% of participating nurses are interested in a template letter to assist in achieving immunization compliance in their schools. In response, Penn State PRO Wellness has created the Immunization Compliance Notification Letter template for nurses to assist with communicating to families regarding their children’s vaccination needs.
Click here to complete the Immunization Notification Letter request form, be sure to select ‘Immunization Letter’ from the selection options. Once your information is received, you will gain access to our Immunization Letter via email.
Dermatology - Rashes: Is it contagious?
View VideoMental Health - Depression, Anxiety and Medications
View VideoTeen Health: Mental Health
View VideoDiabetes - Management of Childhood Diabetes in School
View VideoAsthma and Allergic Rhinitis
View VideoManagement of Food Allergies
View VideoTeen Health: Violence Prevention
View VideoTeen Health: Preventive Care
View VideoBMI and You
View VideoOverweight and Obese
View VideoTeen Health: Sexual Health
View VideoTeen Health: Substance Use and Abuse
View VideoBreak the Germ Cycle Infographic
DownloadBe Mindful Infographic
DownloadHealthy Study Habits Infographic
DownloadRise & Sunshine
DownloadTeen Health: Preventive Care Infographic
DownloadTeen Health: Mental Health Infographic
DownloadTeen Health: Sexual Health Infographic
DownloadTeen Health: Substance Use and Abuse Infographic
DownloadTeen Health: Violence Prevention Infographic
DownloadTurn Your Emotions Inside Out Infographic
DownloadHealthy Choices: Eating Healthy on a Budget (English)
DownloadHealthy Choices: Energy Balance
DownloadHealthy Choices: Cooking, Kid Approved (English)
DownloadHealthy Choices: Snack Swaps (English)
DownloadHealthy Choices: Portion Distortion (English)
DownloadHealthy Choices: Rethink Your Drink (English)
DownloadHealthy Choices: Daily Breakfast Tips (English)
DownloadHealthy Choices: Setting Wellness Goals (English)
DownloadHealthy Choices: Getting a Good Night’s Sleep (English)
DownloadHealthy Choices: Family Exercise without Equipment (English)
DownloadHealthy Choices: Eating Healthy on a Budget (Spanish)
DownloadHealthy Choices: Cooking, Kid Approved (Spanish)
DownloadHealthy Choices: Snack Swaps (Spanish)
DownloadHealthy Choices: Portion Distortion (Spanish)
DownloadHealthy Choices: Rethink Your Drink (Spanish)
DownloadHealthy Choices: Daily Breakfast Tips (Spanish)
DownloadHealthy Choices: Setting Wellness Goals (Spanish)
DownloadHealthy Choices: Getting a Good Night’s Sleep (Spanish)
DownloadHealthy Choices: Family Exercise without Equipment (Spanish)
DownloadCDC – Food Allergies in Schools Toolkit
CDC’s toolkit contains tip sheets, training presentations, and podcasts to help school staff implement the Voluntary Guidelines for Managing Food Allergies in order to prevent and manage severe allergic reactions in schools.
View ResourceCDC – Help for Health Insurance
Access a fact sheet to aid schools in helping children and their families enroll in a health insurance plan. Ensuring children have health insurance ensures healthy kids who are more likely to complete high school and even graduate from college.
View ResourceKognito Change Talk
Healthcare providers can change the conversation about childhood obesity by building motivational interviewing skills with this digital practice tool. Engage in a conversation with a virtual mother and her son and apply motivational interviewing techniques to drive positive change in health behaviors.
View ResourceNational Program for Playground Safety (NPPS)
NPPS online courses provide a supportive learning environment where students will have virtual access to instructors that foster dialogue and challenge thinking through interactive, online discussion boards, learning modules, and assignments. All courses are self-driven, allowing learners to complete the course at their own pace.
View ResourceSchool-Based Health Alliance
View resources on common issues related to health and learning, and tools that will help school health providers develop and run high-quality services to serve the health needs of their students.
View Resource